We have published a more recent review of this organization. See our most recent report on the SCI Foundation, formerly known as the Schistosomiasis Control InitiativeI.
More information:
Published: November 2012
Summary
The Schistosomiasis Control Initiative (SCI) assists African governments with treatment of neglected tropical diseases and runs a number of smaller-scale projects (more).
SCI is a recommended organization because of its:
- Focus on a program with a strong track record and excellent cost-effectiveness (more).
- Demonstrated results - the research we have seen suggests that programs SCI has been involved with have been successful in reducing the prevalence of infection in the areas studied (more).
- Room for more funding - SCI has told us that it can use additional funding to expand its core programs and has committed to reporting on how additional funds are used and what results are achieved (more).
Our full review, below, discusses our full assessment of SCI, including what we see as its strengths and weaknesses as well as issues we have yet to resolve.
Our review process
We began reviewing SCI in 2009. Our review has consisted of:
- Reviewing published studies on SCI's programs.
- Extensive communications with SCI Director Alan Fenwick to discuss SCI's methods and funding needs, as well as meetings with other staff at SCI's headquarters in London.
- Requesting and reviewing SCI internal financial and organizational documents.
- Visiting a national schistosomiasis control program meeting and demonstration mass drug administration in Malawi (notes and photos from this visit)
- Following SCI's progress and plans for funds raised as a result of GiveWell's recommendation (see our updates on SCI's progress).
All content on the Schistosomiasis Control Initiative, including past reviews, updates, blog posts and conversation notes, is available here.
Table of Contents
- Summary
- What do they do?
- Does it work?
- What do you get for your dollar?
- Room for more funds?
- SCI as an organization
- Financials
- Unresolved issues
- Sources
What do they do?
SCI works with governments in sub-Saharan Africa to create or scale up mass drug administration programs for neglected tropical diseases (NTD), particularly schistosomiasis and soil-transmitted helminths (STHs), in school-aged children and other groups determined to be at high risk.1 SCI's role has primarily been to solicit grants from large funders, identify country recipients, provide funding to governments for government-implemented programs, provide advisory support, and conduct research on the process and outcomes of the programs.
SCI does not report a comprehensive budget of all of its expenditures. It reports spending for each of its "accounts." It has accounts for each of the grants it has received, as well as accounts for unrestricted donations. We have seen spending details for some of these accounts, including all of the accounts containing unrestricted funds.
Large grants for mass drug administrations
SCI's work has been driven by a number of large grants, each with somewhat varied program designs and geographic coverage:
- Initial Gates Foundation grant: SCI was founded in 2002 through a $32 million grant from the Gates Foundation.2 This grant was used to create national treatment programs for schistosomiasis and soil-transmitted helminths (STHs) in six countries.3
- Grants for integrated NTD control: In 2006, SCI received large grants from USAID and the Gates Foundation to support integrated NTD programs in eight countries for five years to treat lymphatic filariasis, onchocerciasis, and trachoma, in addition to schistosomiasis and STHs.4 It received a grant in 2007 to expand its advisory work to Rwanda and Burundi.5 All of these grants were due to be completed in 2011.6
- DFID grant: In 2010, SCI received funding from the UK's Department for International Development for treating schistosomiasis and soil-transmitted helminths7 in eight countries over five years.8 Other NTDs are not covered by the grant, though DFID also provided funding to the Liverpool School of Tropical Medicine to integrate treatment for lymphatic filariasis with SCI-funded schistosomiasis and STH programs in six countries.9
SCI's role in mass drug administrations in general is to:10
- Advocate for the benefits of mass drug distributions to government officials.
- Assist with planning and fund raising.
- Deliver funding and drugs to governments.
- Provide financial management and technical support.
- Develop procedures for monitoring and evaluation.
Programs funded with unrestricted funds
Prior to 2011, unrestricted funds accounted for a very small portion of SCI's total funding.11 SCI told us that this funding was primarily used to fund treatments in regions of Cote d'Ivoire and Mozambique.12
In part due to GiveWell's recommendation, between November 2011 and October 2012, SCI received about $2 million. Over the same period it spent about $637,000 and made spending commitments totaling $1.37 million (details in our November 2012 update). SCI told us that it has spent (and plans to spend) these funds in three main categories:13
- Starting new deworming programs in countries where SCI has not worked before. SCI hopes that by using unrestricted funds to get national treatment programs started in these countries, it will attract large grants from major donors, such as the UK's Department for International Development (DFID), to continue the programs.
- Supplementing restricted funding in the set of countries supported by a grant from DFID.
- Funding a variety of organizational costs including the salary of a staff member and staff travel.
Other projects
In addition, SCI has received some smaller grants for a variety of projects, including:
- Research. SCI has received a number of smaller grants to carry out research related to NTD control.14
- NTD treatment programs funded by individuals. SCI has received restricted funds from individuals to fund treatment in Uganda (on islands in Lake Victoria) and Burundi.15
- Other NTD-related activities. SCI has also used funding from individuals for surgeries for hydrocele (a symptom of lymphatic filariasis) in Niger, and health education and water and sanitation programs in Burundi.16
Overall spending breakdown
We have seen a number of spending breakdowns from SCI, which vary in the amount of detail, the categories used, and the funding sources or years covered. We do not feel that any one source gives a comprehensive picture of how SCI has spent its money, so we present a few different breakdowns of SCI's expenditures:
- SCI provided a high-level breakdown of spending between its founding in 2002 and April 2010. In this period, SCI spent a total of $68.2 million, of which 59% was spent on country programs (we do not know what this includes), 28% on drugs, 9% on salaries, and 5% on "OHD/College contribution" (our understanding is that this is an administrative fee charged by the college that hosts SCI).17
- SCI also provided spending data for grants that were active as of April 2010 (the integrated NTD control grants discussed above). In aggregate, 48% of this funding had been transferred to governments,18 26% spent on "lab and works supplies," 12% spent on staff, 6% spent on overheads, and 8% spent on various other expenses.19
- For the one grant for which we have line-by-line transaction information, a Gates Foundation grant for Burkina Faso for 2006-2011, 70% was granted to the local NTD organization RISEAL and an additional 27% was spent on drugs and medical supplies.20
- As of January 2011 (the most recent report we have of SCI's full historical funding sources), SCI had received a total of $108 million over the course of its history, of which $42.6 million was from the Gates Foundation (39%), $16.7 million from the U.S. government through USAID (15%), and $38.3 million from the British government through DFID (35%).21 As discussed above, these grants have funded national treatment programs. As of July 2011 (the most recent report we have on donations from individuals), SCI had raised about £850,000 (about $1.31 million) from individuals.22
- As discussed above, SCI has provided details of how it has spent unrestricted funds as of November 2012. See our November 2012 update.
Does it work?
SCI's mass drug administration programs are focused on delivering treatments that have been both (a) independently studied in rigorous trials and found to be effective, and (b) found to be effective in three national programs aided by SCI.
We have remaining concerns about whether the results found in SCI-aided programs are:
- representative of overall results in those countries. The studies only cover the first year or two of the program, and there are a number of ways in which the results may be biased (more
- representative of results in all SCI-aided countries (more). We have only seen detailed results for three of the countries SCI has worked in.
- representative of results that would be achieved with donations from individuals. Donations from individuals may support smaller-scale programs, and we have not seen results from these programs (more).
We also have remaining questions about how many treatments are needed to have lasting impact, and how many treatments each individual receives in SCI's programs (more).
Independent evidence of program effectiveness
SCI's primary program is mass deworming, which we discuss extensively on another page. There is a very strong case that mass deworming is effective in reducing infections. The evidence on the connection to positive quality-of-life impacts is less clear, but there is a possibility that deworming is strongly beneficial.
Internal monitoring: large-scale programs
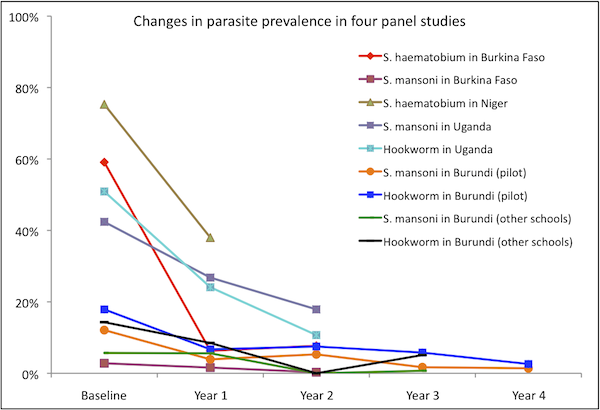
We have seen detailed technical reports for four countries: Burkina Faso, Niger, Uganda, and Burundi. The first three countries accounted for about 74% of SCI funding as of April 2010 (the most recent report we've seen that breaks down overall spending by country),23 though the data below covers only the first year or two of these programs, which started in 2003-2004 and have continued until at least 2010. We also include Burundi for which we have seen a technical report that appears to cover the full time period of SCI's work in the country. Burundi is the only country for which we have seen data on a program that was not funded by SCI's first Gates Foundation grant. Note that the data from Burundi is from two studies: (a) 2007-2011 results from schools included in a pilot program in three provinces; and (b) 2008, 2009, and 2011 results from schools in the other districts.
We focus on these countries because (a) these countries account for the bulk of SCI's spending prior to April 2010 (and evaluations from more recently-funded countries are not yet available) and (b) we have the most in-depth information on them.
Results from Burkina Faso, Niger, Uganda, and Burundi
All of the following data is from uncontrolled panel studies, i.e. the same individuals were examined before and after treatment and the changes in their disease status reported as the effect of the treatment. Cross-sectional studies of children in the same schools as the cohort children and selected to match, in age and sex, the cohort group were also conducted in Burkina Faso with roughly similar results.24 In the four countries, significant decreases in parasite prevalence and intensity, anemia, and some disease manifestations were observed. All of the changes reported in the below table are statistically significant at p<0.05.25
| Schistosoma haematobium | Schistosoma mansoni | Hookworm | ||||
|---|---|---|---|---|---|---|
| Country | Changes in prevalence | Changes in intensity | Changes in prevalence | Changes in intensity | Changes in prevalence | Changes in intensity |
| Burkina Faso | 59.1% at baseline to 7.7% at two years | 94.2 eggs/10ml urine at baseline to 6.8 at two years | 2.8% at baseline to 0.3% at two years | 4.6 eggs per gram of feces at baseline to 0.6 at two years | Not reported | Not reported |
| Niger | 75.3% at baseline to 28% at one year | 22.8% prevalence of heavy-intensity infections at baseline to 4.6% at one year | Not reported | Not reported | Not reported | Not reported |
| Uganda | Not reported (SCI reports very low baseline prevalence26 ) | N/A | 42.4% at baseline to 17.9% at two years | 219.6 eggs per gram of feces at baseline to 37.4 at two years | 50.9% at baseline to 10.7% at two years | 309.4 eggs per gram of feces at baseline to 21.9 at two years |
| Burundi (pilot) | Not reported (SCI reports very low baseline prevalence27 ) | N/A | 12.7% at baseline to 1.7% at four years | Not reported | 17.8% at baseline to 2.7% at four years | Not reported |
| Burundi (other schools) | Not reported (SCI reports very low baseline prevalence28 ) | N/A | 6.2% at baseline to 0.7% at three years | Not reported | 15.1% at baseline to 5.4% at three years | Not reported |
For the other two prominent soil-transmitted helminths, ascaris and trichuris, very low prevalence of ascaris was reported in the Niger and Burkina Faso studies,29 and low baseline levels with modest decreases at two years were reported for both ascaris and trichuris in Uganda. In Burundi, effects on ascaris and trichuris appear inconsistent; prevalence both rose and fell by statistically significant amounts over the five years of the study (with the exception of trichuris, where the rise in prevalence was not statistically significant). Data from Uganda and Burundi are given in the footnote.30
| Country | Anemia | Mean hemoglobin concentration31 | Blood in urine32 | Ultrasound abnormalities of the urinary tract prevalence | Ultrasound abnormalities of the bladder | Thinness or wasting | Shortness or stunting | Firm or hard liver | Firm or hard spleen |
|---|---|---|---|---|---|---|---|---|---|
| Burkina Faso | 65.75% at baseline to 61.59% at one year | 10.97 g/dL at baseline to 11.25 g/dL at one year | Micro: 49.56% at baseline to 10.50% at one year | Not reported | Not reported | Not statistically significant | Not statistically significant | Not reported | Not reported |
| Niger | 61.9% at baseline to 50.4% at one year | 11.0 g/dL at baseline to 11.4 g/dL at one year | Gross: 7.1% at baseline to 0.4% at one year; Micro: 53.5% at baseline to 6.0% at one year | 45.6% at baseline to 15.2% at one year | 41.6% at baseline to 14.7% at one year | Not reported | Not reported | Not reported | Not reported |
| Uganda | 51.6% at baseline to 36.2% at two years | 11.4 g/dL at baseline to 12.0 g/dL at two years | Not reported | Not reported | Not reported | Not reported | Not reported | 63.3% at baseline to 0.8% at two years | 61.6% at basline to 14.1% at one year |
| Burundi (pilot) | 25.4% at baseline to 8.3% at four years | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Burundi (other schools) | 26.0% at baseline to 16.3% at three years | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
Potential issues with the above data
Due to the way in which they were carried out, these studies may overestimate SCI's impact. Potential sources of bias include:
- Monitoring of selected locations. It appears that the authors of the studies we've seen selectively chose locations to monitor, rather than examining a representative sample of treated areas.
- In Burkina Faso, monitoring occurred in four out of 13 regions that received treatment. These four regions were selected because they were "known a priori to be places where schistosomiasis is highly endemic."33
- In Niger, survey locations were stratified "to represent the two main transmission patterns in Niger," and all of the survey locations were located near bodies of water.34 SCI told us that these locations "are not representative of the treatment population as a whole. They were selected to indicate the impact of treatment in schools with varying prevalence and intensity of both [types of schistosomiasis]."35
- In Uganda, as in Niger, survey locations "were selected to represent different transmission settings."36
- In Burundi, pilot program "schools were chosen based on 3 zones; each containing different NTD endemicity": the "STHs + Schistosomiasis + onchocerciasis" zone, the "STHs +onchocerciasis" zone, and the "STH only endemic areas."37 For the survey of non-pilot program schools, the report we have seen says only, "The selection of schools was done randomly from the non-pilot provinces; taking into account 11 separate ecological zones."38
- Low follow up rates. Follow up rates tended to be quite low (43-73% over two years of study).39
SCI stated to us that the children that were available for follow up in most or all of the above studies were those children who had not dropped out of school and were not absent on the given day.40
There are a few ways in which this phenomenon could lead to overstatement of effectiveness:
- If schistosomiasis itself contributes to dropping out of school, then the children who are successfully followed up with may be the ones who are most likely to have ceased being infected for reasons unrelated to treatment.
- A similar dynamic could hold if a third factor (for example, low family income or poor hygiene) contributes to both schistosomiasis infection and dropping out of school.
- The children who are successfully found, year after year, seem (intuitively speaking) more likely to be the same children who are successfully treated, year after year. Therefore, effects of treatment on these children aren't necessarily representative of effects on the treated population as a whole.
The baseline characteristics measured in the studies did differ in some ways between those children who were found on follow up and those who were not; however the differences do not exhibit consistent patterns across the three studies (not reported for Burundi).41
- Possibility of unreported measured results. As seen in the above tables, many results are reported for one or two but not all of the countries. It is possible that some of these indicators were measured but not reported in the published studies because they did not show favorable results. This is a speculation only; we have not discussed this question with the studies' authors.
Do these results apply to SCI's large-scale programs generally?
We have limited information on whether the results presented above from Burkina Faso, Niger, Uganda, and Burundi can be generalized to other countries in which SCI has run programs (see footnote for details of where SCI has worked over what years and what results we have seen42 ). In addition to the published studies discussed above, we requested monitoring reports from Tanzania, which we did not receive.
For its first year or two of work in Mali and Tanzania, SCI posts results, but not details of how the data was collected, on its website. While reported results show positive effects, results are not reported for many indicators and we do not know if the methods used to collect this data were highly rigorous.43
SCI notes that in Zambia, which received support under SCI's initial Gates Foundation grant, implementation was poor and results below expectations.44
We have not seen evaluations of SCI's work on diseases other than schistosomiasis and soil-transmitted helminths and our understanding from conversations with SCI is that it does not monitor these programs. We have not seen evaluations of SCI's work with populations other than schoolchildren. Adults also receive treatment in some SCI-funded programs.45
Internal monitoring: activities funded with unrestricted funds
We have seen limited information on the success of activities SCI has funded with unrestricted funds:
- We have seen a list of treatments given by community in Mozambique in 2008,46 and a narrative report (undated; we received it in 2011) that states, "Since 2006 surveying and treatment has taken place in 14 of the district’s primary schools, in which every child is administered with the correct dosage of Albendazole and Praziquantel annually."47
- We have not seen monitoring from the pilot project in Cote d'Ivoire. The country is now receiving funding from DFID and SCI plans to conduct regular monitoring there in the future (see our November 2012 update).
- SCI has shared non-public reports from staff members' visits to a number of countries (see our November 2012 update).
- SCI shared a government report on the distribution in Senegal in early 2012, which provides treatment coverage data for part of the area that received SCI-funded treatments and notes that not all data is available because some has been withheld by health workers who are involved in a labor dispute.48
- We have seen monitoring plans for the eight countries in which DFID began funding schistosomiasis control in 2011-2012, many of which have also received unrestricted funding from SCI (see our November 2012 update).
As of this writing in November 2012, we do not yet expect monitoring from countries where SCI is working to start new national deworming programs (Ethiopia, Zimbabwe and Mauritania) with unrestricted funds, as treatments have not yet started in those countries.49
Possible negative and offsetting impact
- Concerns over whether treatment was sustained: We believe it is important that deworming programs are sustained over time, as re-infection is rapid and a one-time treatment may have little long-term effect.50
SCI told us that it "is hesitant to use one-off donations to fund programs that couldn't be continued over the long run,"51
and seems to have a reasonable record of maintaining national programs over time.52
However, it is not clear to us (a) how likely programs funded by individual donors are to be sustained after the first few years; (b) the extent to which SCI-funded programs have succeeded in treating the same children multiple times, as opposed to simply treating the same areas multiple times (and thus treating different children once each).
We remain unsure about how many treatments are needed to impact health. SCI told us that its views on what groups should be treated and how often "is largely based on intuition and common sense, though it usually works and SCI collects sufficient data to know when it isn't working. In general, in high endemicity areas re-infection is a major issue; in lower endemicity areas, a single treatment can be sufficient."53 One example of the variation in treatment patterns is what SCI told us about its program in Yemen:
SCI distinguishes between high, medium and low prevalence areas. In high prevalence areas, SCI treats the whole population once, and children for five years. In medium prevalence areas, SCI treats the whole population once, and children every other year. In low prevalence areas, SCI treats children every other year.54
- Replacement of government funding: In the past, SCI has largely supported programs that did not exist before its support.55 We have not seen data on government spending on NTDs before and after receiving SCI support.
- Diversion of skilled labor: Drug distribution occurs only once or twice per year and appears to be conducted by teachers, community drug distributors (who receive minimal training to fulfill this role), and health center staff.56 Given the limited time and skill demands of mass drug distribution,57 we are not highly concerned about distorted incentives for skilled professionals.
What do you get for your dollar?
The details of our calculation of SCI's full cost per treatment are in this spreadsheet. In short, using data on the value of SCI's grants from 2002-2010, the number of schistosomiasis and STH treatments it reports delivering during that period, and conversations with SCI about how the grants were used, we estimate:
- The upper-bound on the cost per treatment during this period was $0.79. This includes all grants received in "SCI's costs," with the exception of the DFID grant which was awarded in late 2010.
- Our best guess excludes a few more grants that, based on conversations with SCI, we believe can reasonably be excluded from the cost of treatment. This best guess is intended to be fairly conservative. Under these assumptions, we estimate the cost per treatment at $0.68.
- A less conservative estimate, that attempts to subtract out research costs that SCI told us were above and beyond normal monitoring and evaluation costs, yields $0.49 per treatment.
- A forward-looking estimate based on the funding received from DFID and the number of treatments committed under that grant, yields an expected cost of additional treatments of $0.51 (officially 3 treatments per 1 GBP), though (a) this does not include costs such as organizational overhead and (b) SCI notes that it is possible that this funding will be supplemented with other funding to achieve the treatment goals.
Note that SCI's USAID grants involved some treatments for diseases other than schistosomiasis and STHs; we do not include these on either side of the calculation, i.e., we do not include the treatments in the denominator of "cost per treatment" or the value of donated drugs in the numerator of "cost per treatment."
We discuss how the above figures relate to how much it costs to improve a child's health and development at our report on mass treatment programs for schistosomiasis and STHs.
Room for more funds?
As of November 2012, SCI held about $840,000 in unallocated funds. SCI is considering using this funding and additional funds it raises on some combination of the following. We note that SCI's plans have been somewhat fluid to date. We do not consider this a bad thing and have encouraged unrestricted funding to allow SCI flexibility.
- Fund additional treatments in Ethiopia. SCI has spent about $51,000 in the country and committed an additional $711,000 to deliver 1.5 million treatments of donated praziquantel to school children to treat schistosomiasis and 6.8 million treatments donated mebendazole to school children to treat soil-transmitted helminths.58 It is not clear to us whether additional unrestricted funds or how much unrestricted funding will be needed in Ethiopia; SCI has told us that it hopes to secure funding in the future for Ethiopia from DFID.59 SCI notes, "The estimated need for Ethiopia over the next 6 years may be as high as $60 million."60
- Starting a national program in Zimbabawe. SCI has committed unrestricted funding for disease mapping and baseline data collection in the country.61
- Expanding DFID-funded programs in Cote d'Ivoire, Mozambique, Malawi, and Tanzania. SCI believes that DFID funding will not be sufficient to reach national coverage in these countries.62
SCI as an organization
We believe the Schistosomiasis Control Initiative to be a strong and effective organization overall.
- Track record: SCI has a long and impressive track record; it has consistently gotten national deworming programs to go through and (as discussed above) to successfully reduce worm prevalence rates.
- Self-evaluation: SCI’s self-evaluation is among the best we’ve seen from any organization. That said, it has generally been done by academics and SCI hasn’t always been able to provide the details of what was done (and thus to answer concerns about possible weaknesses in the evaluations), and we have not seen evaluations from more recent programs. In addition, we differ strongly on the strength of the evidential case for deworming (see our 2012 post on deworming and the comments that follow it).
- Transparency: SCI has consistently been strong in its commitment to transparency. It has provided all the information we’ve asked for and has never hesitated to share it publicly (unless it had what we felt was a good reason). It has allowed a lot of public dialogue that other charities may have been uncomfortable with.
- Communication: We don’t feel that SCI has ever purposefully been indirect with us, but we have often struggled to communicate effectively with SCI representatives, and we still are not as clear on some issues as we'd like to be (more at our most recent update on SCI).
More on how we think about evaluating organizations at our 2012 blog post.
Financials
We discuss SCI's financials above.
Unresolved issues
While we believe that SCI is an outstanding organization, we list some unresolved issues below:
- As discussed in detail above, we have remaining concerns about SCI's evidence of effectiveness. While studies have implied success in reducing the prevalence of infection, we are concerned about how relevant the studied populations are to the full populations treated by the programs.
- Though we have researched the effect of schistosomiasis and STH infection on short- and long-term health, we lack confidence in the severity and frequency of symptoms. Based on the information we have seen, it seems that these infections cause little harm in most cases, but can cause moderate to severe long-term damage in a small percentage of cases.
- SCI's future funding priorities include activities whose likely impact is unclear to us, including treating adults and advocacy.
Sources
- 1
"Objectives of SCI
- To encourage development of sustainable schistosomiasis and STH control programmes in sub-Saharan Africa.
- In the selected countries: to reach at least 75% of school-aged children (which in most countries would be from 6 to 15-year-old) and other high-risk groups with chemotherapy, namely PZQ and ALB; and thereby reducing prevalence and intensity of schistosomiasis and STH infections; as well as reducing schistosomiasis-related morbidity in high risk groups; and burdens due to STH infections in the targeted populations.
- To create a demand for sustained schistosomiasis and STH control.
- To promote access to anthelminthic drugs and good case management in the regular health system.
- To develop a rigorous monitoring and evaluation plan which will generate the information required to determine whether or not the objectives have been met."
Fenwick et al. 2009, Pg 3.
- 2
"The move towards national control programmes in sub-Saharan Africa was facilitated by an award from the Bill and Melinda Gates Foundation (BMGF; http://www.gatesfoundation.org) Global Health Program in 2002, to the SCI for the implementation and evaluation of control of schistosomiasis." Fenwick et al. 2009, Pg 2. Amount at Gates Foundation Imperial College London (June 2002).
- 3
"Six countries were selected by October 2003 for full support: Burkina Faso, Mali, Niger, Uganda, Tanzania and Zambia. The countries each proposed a different implementation approach and management structure for their large-scale schistosomiasis control. This was readily accepted because the BMGF required SCI to test the ‘proof-of-principle’ of national scale, Ministry of Health (MoH)-led schistosomiasis control programmes. SCI is based in Imperial College London and operated with the principle that all programmes were country owned and run, with SCI staff offering technical and other assistance, but not as expatriates living in-country. Programmes were based in the MoH in the respective country, and SCI offered support to improve the national health system." Fenwick et al. 2009, Pg 2.
Between 2003 and 2008, SCI provided treatment for schistosomiasis and soil-transmitted helminths to the following number of people (Fenwick et al. 2009, Pg 3, Table 1).
Number treated by country (millions) Year Uganda Burkina Faso Niger Mali Tanzania Zambia 2003 0.43 - - - 0.10 - 2004 1.23 1.03 0.67 - 0.44 - 2005 2.99 2.30 2.01 2.60 2.95 - 2006 1.51 2.82 1.56 2.18 0.38 0.56 2007 1.81 0.75 2.07 0.65 2.65 0.25 2008 1.50 2.70 5.28 - 1.24 - - 4
"Current and future rounds of treatment in all six countries are being delivered in an integrated manner to include schistosomiasis, STH, lymphatic filariasis, onchocerciasis and trachoma." Fenwick et al. 2009, Pg 10. The "six countries" refers to the six countries funded by SCI's first Gates Foundation grant.
Countries and dates from Schistosomiasis Control Initiative, Board management accounts (April 2010) - 5
Schistosomiasis Control Initiative, Burundi: Impact
Schistosomiasis Control Initiative, Rwanda: Strategy
Schistosomiasis Control Initiative, Board management accounts (April 2010) - 6
Schistosomiasis Control Initiative, Account summary (May 2011)
- 7
"A team from Imperial College London has been awarded 25 million funding from the UK Government to continue its fight against neglected tropical diseases, it was announced this week. The money will enable the Schistosomiasis Control Initiative (SCI) to provide 75 million treatments to protect some of the world’s poorest children against schistosomiasis – an illness caused by parasitic worms – and soil-transmitted helminths (STH). £15 million of the funding will be spent directly on procuring drug treatments, through an organisation called Crown Agents. The rest will be administered by SCI." Schistosomiasis Control Initiative, Imperial initiative to protect children from tropical disease awarded ₤25m government backing.
- 8
Alan Fenwick, SCI Director, conversation with GiveWell, October 17, 2011.
- 9
"SCI will be assisted in their drug delivery by the Centre for Neglected Tropical Diseases at Liverpool School of Tropical Medicine via a sub contract through LATH (Liverpool Associates in Tropical Health). In six countries, this will lead to treatment for lymphatic filariasis – another worm disease – becoming integrated with schistosomiasis and STH treatment." Schistosomiasis Control Initiative, Imperial initiative to protect children from tropical disease awarded ₤25m government backing.
- 10
- Alan Fenwick, SCI Director, phone conversation with GiveWell, June 17, 2010.
- Schistosomiasis Control Initiative, Summary sheet of treatments instigated and overseen by SCI
- Schistosomiasis Control Initiative, Proposal by SCI, Imperial College to manage the Program for Integrated Control of Neglected Tropical Diseases in Côte d'Ivoire
- 11
As of July 2011, it had received about $580,000 in unrestricted funding (Schistosomiasis Control Initiative, IC Trust summary (September 2011)) and $108 million overall (Schistosomiasis Control Initiative, Gates Foundation final report (January 2011) Pg. 20).
- 12
"For the smaller donor, we have two or three projects, which we have been supporting and which will hopefully lead to pilot project in their respective countries.
- In Cote d'Ivore, we now have funding from the U.K. Department for International Development (DFID). There will eventually be a national program.
- In Mozambique, we have a doctor running a practice for 70,000 people. We have been funding her to test people, do surveys and give drugs to treat people. Up until now, that has taken all the individual funding that comes in."
Alan Fenwick, SCI Director, phone conversation with GiveWell, February 16, 2011.
- 13
See our November 2012 update on SCI.
- 14
SCI's summary of active accounts as of May 2011 lists five research grants totaling £1.9 million, or about $3 million. Schistosomiasis Control Initiative, Account summary (May 2011).
- 15
"Once we have people that want to give at least $100,000, we talk to them directly. Two examples:
- Someone wanted to do something special with his money, so we're doing hydrocele surgery in Niger. He gave us $200,000 and we told him we could do ~1000 hydrocele surgeries.
- Another person was interested in Uganda. So, we identified islands there in Lake Victoria that are relatively accessible and provided treatments there."
Alan Fenwick, SCI Director, phone conversation with GiveWell, February 16, 2011.
Funds committed for future use listed in Schistosomiasis Control Initiative, IC Trust summary (September 2011):- Disease prevalence mapping in Cote D'Ivoire (£16,000)
- Shipping donated drugs to Cote D'Ivoire (£50,000)
- Burundi (£640,000). SCI told us that this was being used to continue an mass drug administration program that ran out of funds. Alan Fenwick, SCI Director, phone conversation with GiveWell, September 15, 2011.
- Unspecified activities in Yemen (£100,000) and Senegal (£30,000)
- Hydrocoele treatments in Niger (£25,000)
- 16
Alan Fenwick, SCI Director, phone conversation with GiveWell, September 15, 2011. Note: "SCI generally doesn't do water and sanitation programs because of the expense. In Burundi they're doing water and sanitation programming because they have been successful there with running a program and treating schistosomiasis, but soil-transmitted helminth infections remain persistent." Alan Fenwick, SCI Director, conversation with GiveWell, October 17, 2011.
- 17
Schistosomiasis Control Initiative, Board management accounts (April 2010)
"When SCI claims back from USAID, a small % -- about 6% -- is an overhead charge that goes to Imperial College. SCI is not a registered charity but a part of Imperial College." Alan Fenwick, SCI Director, phone conversation with GiveWell, February 16, 2011. - 18
The line item is "external consultants." SCI told us, "The line 'external consultants' which seems a high personnel cost in some sub awards is in fact a transfer to the Countries - which for the sake of Imperial accounting are classed as 'external consultants' because Imperial College accounting system has no line for field work in Africa." Alan Fenwick, SCI Director, email to GiveWell, February 1, 2011.
- 19
Schistosomiasis Control Initiative, Board management accounts (April 2010)
Note that a source covering slightly different dates and grants reported a slightly different breakdown. Aggregating spending data from the Gates Foundation (2006-2011) and USAID (2006-2009) integrated control grants, we estimate that SCI spent about 38% of this funding on "field work expenses," 25% on drugs, 21% on staff, and 17% on various other expenses. We are unclear what "field work expenses" signifies. For the one country for which we have more detail, Burkina Faso, "field work expenses" were grants to the organization RISEAL, which is described on its website as "a federation of associations operating in West Africa, Madagascar, and in Europe" to "promote the control of Neglected Tropical Diseases" (RISEAL Homepage). However, it is our understanding from conversations with SCI that much of its funding is often channeled via governments. Data from Schistosomiasis Control Initiative, Gates2 Burkina Faso spending report, Schistosomiasis Control Initiative, Gates2 Y1 to Y5 accounts and Schistosomiasis Control Initiative, USAID RTI Y1 to Y3 accounts. - 20
Schistosomiasis Control Initiative, Gates2 Burkina Faso spending report
- 21
Schistosomiasis Control Initiative, Gates Foundation final report (January 2011) Pg 20.
- 22
Schistosomiasis Control Initiative, IC Trust summary (September 2011).
- 23
Data on spending by country is from Schistosomiasis Control Initiative, Board management accounts (April 2010) Pg 1. Funding, as of April 2010, was concentrated in Burkina Faso (34% of country-specific funding), Niger (33%), Uganda (10%), Burundi and Rwanda (10%; we don't have data for these countries independently), and Tanzania (7%).
- 24
"In addition to the cohort follow-up, a cross-sectional survey was conducted during the second follow-up (2 years post-treatment), in which a group of children (7–14 years old) outside the original cohort were randomly selected and examined in the sentinel schools. The number, age and sex structures were matched to those in the cohort who were present at the second follow-up in each school. Infection status in these children should represent the quality of treatment in children outside cohorts in schools, to confirm and validate the cohort data, i.e. no preferred treatment was given to cohort children…As in the cohort data, the proportion of heavy [S. haematobium infections was reduced from 25% to just 3.2% (Fig. 2). However, these children outside the cohort did show a slightly higher prevalence and intensity of S. haematobium infection than those in the cohort as in Table 1 (P<0.01) at 2 years post-treatment…In baseline children (7–14 years old) in the original cohort in this region, prevalence of S. mansoni infection was 14.2% (95% CI: 10.8–17.6; n = 408) [13.6% in the cohort baseline] and intensity of infection was 23.0 epg (95% CI: 11.8–34.2; n = 408) [22.4 epg in cohort] before treatment. Two years after treatment, S. mansoni prevalence in this region was 7.6% (95% CI: 4.4–11.0; n = 248) [1.5%in cohort] and intensity of infection was 16.5 epg (95% CI: 1.9–31.0; n = 248) [2.9 epg in cohort] (both P>0.05)." Touré et al. 2008, Pg 781-783.
- 25
Sources for the data in the tables:
- Burkina Faso: Touré et al. 2008 and Koukounari et al. 2007.
- Niger: Tohon et al. 2008.
- Uganda: Kabatereine et al. 2007.
- Burundi: Schistosomiasis Control Initiative, Monitoring and evaluation report for Burundi
- 26"S. haematobium occurs only in a small focus and is of minor public health significance." Kabatereine et al. 2007, Pg 91.
- 27Alan Fenwick, SCI Director, phone conversation with GiveWell, November 28, 2011.
- 28Alan Fenwick, SCI Director, phone conversation with GiveWell, November 28, 2011.
- 29
- "Very low prevalence (0.3 to 0.7%) of Ascaris lumbricoides infection was observed in 5 schools, while 3% of the schoolchildren were infected in 1 school (Sanguile) and no infection was observed in 2 schools (Kaou and Tabalak)." Tohon et al. 2008, Pg 3.
- "For both years examined, Ascaris lumbricoides infection was absent, and the prevalence of Trichuris trichura infection was estimated to be 1.1% at baseline and totally absent 1 year later." Koukounari et al. 2007, Pg 663.
- 30
Results from Kabatereine et al. 2007, Pg 93, Table 2 (see source for 95% confidence intervals) and Schistosomiasis Control Initiative, Monitoring and evaluation report for Burundi (see source for statistical significance). We report "as measured results" for Burundi; SCI also reports model results.
Baseline Year 1 Year 2 Year 3 Year 4 Ascaris in Uganda 2.8% 1.6% 0.6% - - Trichuris in Uganda 2.2% 2.5% 1.6% - - Ascaris in Burundi (pilot) 14.9% 12.9% 20.1% 10.6% 10.1% Trichuris in Burundi (pilot) 3.2% 1.8% 3.9% 1.5% 2.4% Ascaris in Burundi (other schools) 21.6% 11.7% - 9.1% - Trichuris in Burundi (other schools) 10.4% 10.0% - 4.3% - - 31Hemoglobin is a component of blood containing iron. Anemia is defined as a hemoglobin concentrations below an age-dependent threshold.
- 32Gross haematuria: visible blood in the urine; Micro-haematuria: blood in the urine that is detectable by microscopic inspection.
- 33
"The SCI-supported schistosomiasis control program was implemented during 2004 and had treated 3,322,564 school-aged children in the 13 regions of the country through October 2006...For the present study, parasitological and morbidity data were collected from a cohort of 1727 Burkinabé children 6–14 years old, randomly sampled from 16 schools before and 1 year after chemotherapy (2004 and 2005, respectively). The schools included in these surveys were randomly selected from all schools in 4 Regional Health Directorates known a priori to be places where schistosomiasis is highly endemic." Koukounari et al. 2007. Pg 660.
- 34
"Eight villages located in schistosomiasis endemic regions were randomly selected to represent the two main transmission patterns in Niger: six villages located near permanent (Tabalak, Kokorou) or semi-permanent (Kaou, Mozague, Rouafi, and Sabon Birni) ponds and two (Saga Fondo, Sanguile) located along the Niger River. The villages represented the south-western region (Tillabe´ry) and the central-northern region (Tahoua) of the country, with four villages from each region. One village is located in the Sudanian climatic zone and the seven others are in the Sahelian climatic zone." Tohon et al. 2008, Pg 2.
- 35
- 36
Kabatereine et al. 2007, Pg 92.
- 37
Schistosomiasis Control Initiative, Monitoring and evaluation report for Burundi Pg 1.
- 38
Schistosomiasis Control Initiative, Monitoring and evaluation report for Burundi Pg 13.
- 39
- Uganda: "We enrolled 4351 children from 37 schools, of which 2815 (64.7%) were traced and treated at one year follow-up and 1871 (43.0%) at two year follow-up." Kabatereine et al. 2007, Pgs 93-94.
- Burkina Faso: "Of 1727 schoolchildren recruited at baseline, 763 were successfully traced and re-examined at both follow-ups with three complete sets of longitudinal parasitological data on S. haematobium... Among 763 children, 322 had valid data entry for S. mansoni at all three surveys." Touré et al. 2008, Pgs 781-782.
- Niger: "Of the 1656 children recruited at baseline, 1193 (72.04%) were successfully followed-up in both year 1 and year 2 surveys." Schistosomiasis Control Initiative, Niger: Impact
- Burundi: In the pilot program survey, 53.3% of children surveyed at baseline were found for disease prevalence testing at the fourth follow up; however, only 49.6% were found at the first follow up, indicating that not all children found at the fourth follow up were found in all four follow ups. 64.8% were found for anemia testing at the fourth follow up (but only 60.5% at the first follow up). In the other schools survey, 56.5% of children surveyed at baseline were found for disease prevalence testing at the second follow up. 56.7% were found for anemia testing at the fourth follow up. Schistosomiasis Control Initiative, Monitoring and evaluation report for Burundi Pgs 1 and 13.
- 40
Benjamin Styles, SCI Senior Biostatistician, phone conversation with GiveWell, August 12, 2011.
- 41
- Burkina Faso: "Baseline characteristics of children successfully followed-up showed that they had a lower mean age (9.6 years versus 11.0 years; P<0.01), a lower proportion of boys (54.1% versus 59.1%; P<0.05), higher S. haematobium prevalence (59.9% versus 53.1%; P$lt;0.01) but a similar intensity of S. haematobium infection (93.3 e/10 ml versus 91.2 e/10 ml; P<0.05), compared with those who had dropped out." Touré et al. 2008, Pgs 781-782.
- Niger: "Compared to those children who remained in the study cohort, the 216 children who dropped out after the initial survey differed significantly in the prevalence of S. haematobium infection (75.4% vs. 78%, respectively), but had less frequently heavy-intensity infections (22.8% vs. 16.5%, respectively). On the other hand, they did not differ in mean age (8.7 vs. 8.9 years, respectively), in the prevalence of anaemia (61.9% vs. 59.7%, respectively) nor in mean haemoglobinemia (11.04 g/dl vs. 11.03 g/dl, respectively)." Tohon et al. 2008, Pg e241.
- Uganda: "The baseline characteristics did not differ significantly among those included in the evaluation one-year post treatment and those lost to follow-up (see Table 1, available at http://www.who.int). However, we found the prevalence and mean intensity of S. mansoni to be significantly higher among those children who were lost to follow-up compared to those successfully followed up two years post treatment." Kabatereine et al. 2007, Pgs 93-94.
- 42
Funding sources in table below are compiled from:
Schistosomiasis Control Initiative, Summary sheet of treatments instigated and overseen by SCI
Alan Fenwick, SCI Director, phone conversation with GiveWell, June 17, 2010
Schistosomiasis Control Initiative, Board management accounts (April 2010)
Funding for mass treatment | Have we seen disease prevalence/intensity or morbidity results? 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Burkina Faso - Gates | Results with details Gates | Results with details Gates/ USAID | Results with details Gates/ USAID | Results without details Gates/ USAID | No results Gates / USAID | No results Gates / USAID | No results Gates / USAID | No results (Taken over by HKI) Burundi - - - - GNNTDC | Results with details GNNTDC | Results with details GNNTDC | Results with details GNNTDC | Results with details Individual | Results with details Individual | Results expected later Cote D'Ivoire - - - - - - - - DFID | No results yet Liberia - - - - - - - - DFID | No results yet DFID | No results yet Malawi - - - - - - - - DFID | No results yet DFID | No results yet Mali - Gates | Results without details Gates | Results without details Gates/ USAID | Results without details USAID | No results USAID | No results USAID | No results (Taken over by HKI) (Taken over by HKI) Mozambique - - - - - - - - DFID | No results yet DFID | No results yet Niger - Gates | Results with details Gates | Results with details Gates/ USAID | Results without details Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results DFID | No results yet DFID | No results yet Rwanda - - - - GNNTDC | No results GNNTDC | No results GNNTDC | No results GNNTDC | No results ? End Fund | No results yet Tanzania Gates | Results without details Gates | Results without details Gates | No results Gates | No results Gates | No results Gates | No results Gates | No results Gates | No results DFID | No results yet DFID | No results yet Uganda Gates | Results with details Gates | Results with details Gates | Results with details Gates/ USAID | Results without details Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results DFID | No results yet DFID | No results yet Yemen - - - - - - - - Unrestricted SCI funds | No results yet World Bank | No results yet Zambia - Gates | Known failure Gates | Known failure Gates | Known failure Gates | Known failure - - - DFID | No results yet DFID | No results yet - 43
Schistosomiasis Control Initiative, Mali: Impact
Schistosomiasis Control Initiative, Tanzania: ImpactSchistosoma haematobium Schistosoma mansoni Hookworm Anemia Country Follow up rate Changes in prevalence Changes in intensity Changes in prevalence Changes in intensity Changes in prevalence Changes in intensity Changes in prevalence Changes in mean haemoglobinemia Mali 58% over two years About 90% at baseline to about 50% at two years About 30% prevalence of heavy-intensity infections at baseline to about 3% at one year About 21% at baseline to about 13% at two years Not reported About 7% at baseline to about 2% at two years Not reported Not reported Not reported Tanzania 65% at one year Not reported Not reported in aggregate; about 3-52% at basline to 2-10% at follow up Not reported Not reported 39.81% at baseline to about 17.36% at one year Not reported 47.15% at baseline to about 32.97% at one year Not reported - 44
"Zambia has been less successful in reaching its original programme target of expanding coverage to treating 2 million school-aged individuals and had only achieved, according to incompletely reported coverage, around 25% of this target by July 2007." Fenwick et al. 2009, Pg 9.
- 45
"Who has been treated (adults/school children/pre-school children):
Burundi: For STH: children 1-14 yrs, pregnant women under 49 yrs; For schisto: children 5-14 yrs, adults in high prevelance areas…
Malawi: School aged children 4.4 m and adults 1.2 m…
Niger: communities…
Senegal: MDA in April 2012 - private and public schools, islamic schools (called Dahara) and communities…
Uganda: Communities on Lake Victoria islands…
Yemen: Children and adults…
Zimbabwe: Predominantly school aged children but adults if justified."
Schistosomiasis Control Initiative, Program update (September 2012), sheet “By county 2012”. - 46
MANNA Campanha do controle de shistosomiase e parasitoses intestinais (February to June 2008).
- 47
MANNA A firsthand look at the problems and pathways to controlling schistosomiasis in Mozambique.
- 48
"Withholding of the data by the health unionists since 2010. Negotiation was started during the meetings and the great importance of the MDA had was also highlighted as well as the negative consequences the MoH might have to face regarding the future of partnership, in case of not being able to get data and reports."; "Due to health information withholding, it was impossible to collect all data." Government of Senegal Report on MDA (2012) Pgs 10 and 12.
Date of MDA (April 2012) from Schistosomiasis Control Initiative, Program update (September 2012). - 49
See our November 2012 update.
- 50
"Single-dose oral therapies can kill the worms, reducing ... infections by 99 percent ... Reinfection is rapid, however, with worm burden often returning to eighty percent or more of its original level within a year ... and hence geohelminth drugs must be taken every six months and schistosomiasis drugs must be taken annually." Miguel and Kremer 2004, Pg 161.
- 51
Alan Fenwick, SCI Director, conversation with GiveWell, October 17, 2011.
- 52
See table "Funding for mass treatment | Have we seen disease prevalence/intensity or morbidity results?" in previous footnote.
- 53
Alan Fenwick, SCI Director, conversation with GiveWell, October 17, 2011.
- 54
Alan Fenwick, SCI Director, conversation with GiveWell, October 17, 2011.
- 55
- Uganda: "The first country to implement a control programme on a national scale...Uganda implemented the SCI-supported control programme in April 2003." Kabatereine et al. 2007, Pg 91.
- Burkina Faso: "Some small-scale control activities with treatment had taken place in some areas in the past,11,13 but the national control programme did not start until 2004." Touré et al. 2008, Pg 780.
- Niger: "Niger’s National Schistosomiasis and Soil-Transmitted Control Programme (PNLBG) was launched at 2004." Fenwick et al. 2009, Pg 5.
- Mali: "In the following years many planned activities were not implemented due to limited financial resources but finally in 2004 national control activities recommenced in the country with support from the SCI." Fenwick et al. 2009, Pg 5.
- Tanzania: "The failure to embrace a national treatment programme has been due primarily to the costs involved in reaching the millions of individuals estimated to be at risk of infection, and the Ministry of Health was never able to support treatment within their budget. In October 2003, the Tanzanian National Plan was approved for funding by the SCI as a step towards developing a sustainable control programme." Kabatereine et al. 2006, Pg 334.
- Zambia: "'The Zambian Bilharzia Control Programme' (ZBCP) was established in 2004 to develop a MoH and MoE joint strategy for bilharzia and worm control. The MoE was already in receipt of a grant from the United States Agency for Inter- national Development (USAID) for implementing training and treatment in some schools on a small scale in two provinces, Eastern and Southern, which was known as the ‘School Health and Nutrition programme’ (SHN)." Fenwick et al. 2009, Pg 4.
- 56
"Drug distribution channels:
- School-based delivery for school children. School teachers will be trained to carry out drug distribution at schools.
- Community-based delivery for school-aged children who are not attending school and for community adults at high risk. Community Drug Distributors (CDD) will be trained to deliver the drugs at community.
- Health centre-based delivery. Drugs will be made available at health centres for those in the community who do not qualify for MDA and who request for treatment. Health workers at the centres will be trained.
Drug distributors need a minimum of one day’s training to understand the basis for calculating dosages, the necessary actions to deal with side-effects and treatment record keeping and reporting." Schistosomiasis Control Initiative, Neglected tropical diseases in Mozambique, Pg 23.
"For schistosomiasis and STHs, treatment will be conducted through schools by the teachers. For LF, treatment will be conducted through community directed treatment, by the CDDs and community health agents, managed by the district medical officer." Schistosomiasis Control Initiative, Proposal by SCI, Imperial College to manage the Program for Integrated Control of Neglected Tropical Diseases in Côte d'Ivoire, Pg 23. - 57
See our overview of priority programs.
- 58
GiveWell SCI financial details and summary (November 2011 to October 2012), Sheet Summary.
- 59
Alan Fenwick, SCI Director, phone conversation with GiveWell, August 13, 2012.
- 60
Schistosomiasis Control Initiative, Program update (September 2012), Sheet “By country plans”.
- 61
GiveWell SCI financial details and summary (November 2011 to October 2012), Sheet Summary.
- 62
Schistosomiasis Control Initiative, Program update (September 2012), Sheet “By country plans”.
